Anomaly + Fraud Detection
Identifying Medicaid Fraud
RS21 works with agencies to provide computer-assisted audit techniques that allow teams of forensic accountants to more efficiently search claims databases for suspicious billing activity.
Analytic approaches – from rule-based flagging to complex machine learning models – afford improved efficiency by focusing an investigator’s attention on cases that are most likely to be fraudulent.
Investigator Dashboard Concept
Fraud, Abuse, and Waste in Medicaid
“$860 million in fraudulent Medicaid claims were recovered across the United States in 2018. This equates to approximately $14 for every $10,000 in Medicaid expenditure.
The money lost due to fraudulent activity places enormous financial strain on federal and state healthcare programs, diverting precious resources away from those who need them.”
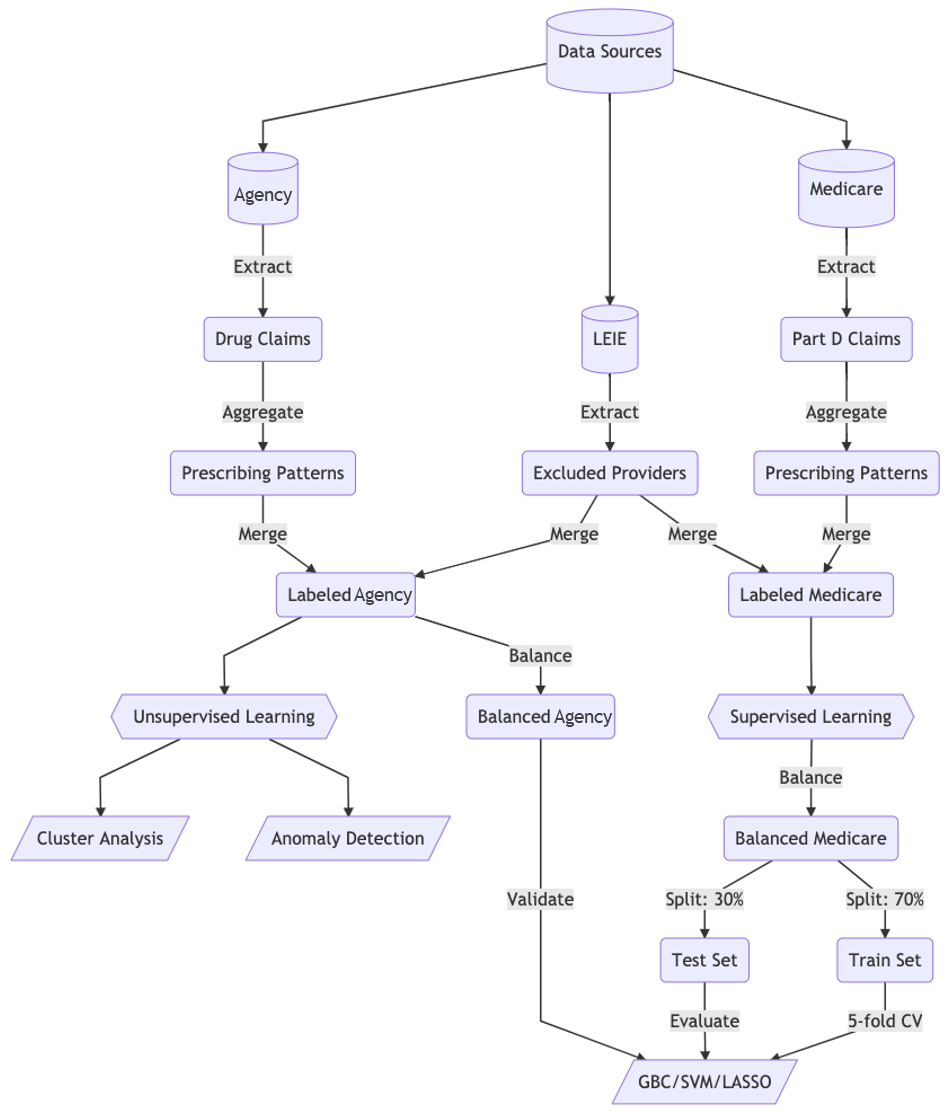
Analytics Pipeline
A Machine Learning Solution
RS21 applies machine learning algorithms to analyze Medicaid Claims Data and identify suspected fraud. The majority of known fraudulent providers are identifiable by our models as outliers when analyzing an agency’s multidimensional data.
Multiple anomaly detection models “vote” on whether a provider is an outlier and allows investigators to work off a prioritized list of potential fraudulent actors.
Additionally, we work with agencies to improve data models to dramatically reduce the time it takes to query data and to provide investigators with direct access to information.
The combination of using machine learning to target possible fraudulent activity and empowering investigators with direct access to data can increase efficiency and enable public agencies to recover millions of dollars annually in fraudulent Medicaid expenditures.